Role of Third Party Administrators (TPA) in Health Insurance

It is very common to come across individuals who are confused between the insurance company and the Third Party Administrators, commonly known as TPAs. When we ask them who their insurance company is, we often get the name of the TPA as the answer. Hence we decided that we would set the record straight!
Insurance company is the one who insures or covers the risk, in this case the medical risk of an individual. We pay the premium required to cover the risk to the insurance companies. Third Party Administrators on the other hand, are hired by the insurance company to manage its medical claims processing.
The Insurance Regulatory and Development Authority of India (IRDA) introduced TPAs in the year 2001 and defines it s a Third Party Administrator who, for the time being, is licensed by the Authority, and is engaged, for a fee or remuneration, in the agreement with an insurance company, for the provision of health services. Out of the 31 TPAs licensed by IRDA, some of the TPAs functioning across India are TTK Health Services (renamed as Vidal Health), Medi Assist, Health India and so on.
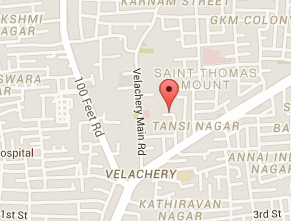
TPAs undertake claims processing, tying up with hospitals across the country to provide cashless hospital facilities and maintaining of claims data for future use by the insurers. In other words, the administration of claims is outsourced to the TPAs by the insurance company. If Third Party Administrators are hired by the insurance company, then their services would be present in individual retail policies as well as corporate group mediclaim policies. TPAs may differ for different branches of the same insurance company. TPAs are the ones who issue the Health Id card that we use while availing cashless benefits.
When you are hospitalized and wish to go for cashless settlement, the hospitals interact with the TPAs to find out whether the patient can be treated and discharged on a cashless basis.
When a reimbursement claim occurs the claim papers have to be submitted to the concerned TPA and not to the insurance company’s branch from where you have purchased the policy. The TPA will scrutinize the papers and either approves the claim or rejects the same based on the policy conditions. The TPA would have the policy wording of all the insurance companies it has tied up with. If the policyholder is not satisfied with the outcome of the claim settlement, the grievances would have to be taken up with the insurance company and not with the TPA.
Coming to private insurance players, most of them have in-house TPA which means that these companies would have a team of doctors and dedicated staff who would be handling the claims. This step is often taken by the insurance company to reduce the cost of administration and in turn the premium that is charged by the company. However, for large public sector insurers, where claim levels are huge, outsourcing the claims settlement would be cheaper than setting up their own claims department.
However, of late, the four public sector insurers have joined hands and have created a TPA called Health Insurance TPA for the purpose of processing claims arising out of Health Insurance policies of insurance companies. It is a joint venture of National Insurance, New India Assurance, Oriental Insurance, United India Insurance and General Insurance Corporation of India. It was supposed to become operational with effect from April 2014. The service efficiency of this TPA is something policyholders would have to wait and experience.
- Log in to post comments